The National Commission on Certification of Physician Assistants® (NCCPA®) maintains a detailed content blueprint for the Physician Assistant National Recertifying Examination (PANRE) and Physician Assistant National Recertifying Longitudinal Assessment (PANRE-LA). This outline covers the allocation of exam questions based on specific content categories and the level of detail at which topics must be understood.
The NCCPA’s recertification exams were revised in 2019 based on feedback from practicing PAs to assess the core medical knowledge necessary for certified PAs. Since then, the PANRE blueprint has been periodically updated to reflect the findings of more recent practice analyses.
Blueprint Categories and Performance Expectations
The NCCPA’s PANRE blueprint is organized by content categories, generally being the different organ systems you’ll need to know. They’re broken down into specific diseases and disorders that are assigned a level at which you must understand them. These levels, or performance expectations, build off each other to logically differentiate possible question types.
- Level 1 — History & Physical: Given a stated/differential condition, you must know the associated signs, symptoms, history, and physical examination components, complications, risk factors for and risks caused by the stated/differential condition.
- Level 2 — Diagnosis: Given the signs, symptoms, history, risk factors, physical examination findings, and/or appropriate study results/interpretations, you must be able to determine the most likely diagnosis.
- Level 3 — Intervention (Basic): You must be able to manage a disease/disorder with a basic/straightforward presentation, including referral to a specialist and complications of the management intervention.
- Level 4 — Intervention (Complex): You must be able to manage a disease/disorder made complex by other factors and/or increasing in severity and complications of management or intervention.
PANRE & PANRE-LA Content Blueprint
The PANRE blueprint is organized by content category and the assessment level of diseases and disorders. Click on each content category to expand the chart.
| Content Category & Percent Allocation* | Performance Expectation | |||
|---|---|---|---|---|
| History & Physical | Diagnosis | Intervention (Basic) | Intervention (Complex) | |
| Abdominal aortic aneurysm | X | X | X | |
| Acute myocardial infarction: non-ST-segment elevation myocardial infarction (NSTEMI) | X | X | X | |
| Acute myocardial infarction: ST-segment elevation myocardial infarction (STEMI) | X | X | X | X |
| Acute myocarditis | X | X | ||
| Acute pericarditis | X | X | ||
| Angina pectoris (stable and unstable angina) | X | X | X | |
| Aortic dissection | X | X | ||
| Arterial embolism/thrombosis | X | X | X | |
| Atrial fibrillation | X | X | X | |
| Atrial flutter | X | X | ||
| Atrioventricular block | X | X | ||
| Bacterial endocarditis | X | X | X | |
| Bradycardia (stable and unstable) | X | X | X | |
| Bundle branch block | X | X | ||
| Cardiac arrest | X | X | X | |
| Cardiac tamponade | X | X | ||
| Cardiogenic shock | X | X | X | |
| Congenital heart disease | X | X | ||
| Coronary artery disease | X | X | X | X |
| Deep venous thrombosis | X | X | X | X |
| Diastolic heart failure | X | X | X | X |
| Dilated cardiomyopathy | X | X | ||
| Dyslipidemia | X | X | X | X |
| Essential hypertension | X | X | X | X |
| Hypertensive emergency | X | X | X | |
| Hypotension | X | X | X | |
| Hypertrophic cardiomyopathy | X | X | ||
| Orthostatic hypotension | X | X | X | |
| Paroxysmal supraventricular tachycardia | X | X | X | |
| Pericardial effusion | X | X | ||
| Peripheral artery disease | X | X | X | X |
| Phlebitis and thrombophlebitis | X | X | X | |
| Premature atrial/ventricular contractions | X | X | ||
| Rheumatic heart disease | X | X | ||
| Secondary hypertension | X | X | X | |
| Systolic heart failure | X | X | X | X |
| Thoracic aortic aneurysm | X | X | ||
| Torsades de pointes | X | X | X | |
| Valvular disorders (regurgitation, prolapse, stenosis) | X | X | ||
| Varicose veins | X | X | X | |
| Venous insufficiency | X | X | X | |
| Ventricular fibrillation | X | X | X | |
| Ventricular tachycardia | X | X | X |
| Acne vulgaris | X | X | X | |
| Actinic keratosis | X | X | X | |
| Alopecia | X | X | ||
| Atopic dermatitis | X | X | X | |
| Basal cell carcinoma | X | X | ||
| Bites (animal, insect, human) | X | X | X | |
| Burns | X | X | X | |
| Cold injuries | X | X | ||
| Contact dermatitis | X | X | X | |
| Dermatophyte infections | X | X | X | |
| Drug eruptions | X | X | X | |
| Erythema multiforme | X | X | ||
| Hidradenitis suppurativa | X | X | X | |
| Lipomas | X | X | ||
| Localized skin infections (cellulitis, erysipelas, abscesses, impetigo, carbuncles, furuncles) | X | X | X | X |
| Melanoma | X | X | X | |
| Molluscum contagiosum | X | X | X | |
| Necrotizing soft-tissue infection | X | X | X | |
| Onychomycosis | X | X | X | |
| Paronychia | X | X | X | |
| Pigmentation disorders (vitiligo, acanthosis, melasma) | X | X | ||
| Pilonidal disease | X | X | X | |
| Pityriasis rosea | X | X | ||
| Psoriasis | X | X | X | |
| Rosacea | X | X | X | |
| Roseola | X | X | ||
| Seborrheic dermatitis | X | X | X | |
| Severe cutaneous adverse reactions (toxic epidermal necrolysis, Stevens-Johnson syndrome, staphylococcal scalded skin syndrome) | X | X | ||
| Skin infestations (scabies, lice) | X | X | X | |
| Squamous cell carcinoma | X | X | ||
| Ulcers (pressure, diabetic) | X | X | X | |
| Urticaria | X | X | X |
| Benign thyroid nodules | X | X | ||
| Cushing syndrome | X | X | ||
| Diabetes insipidus and SIADH | X | X | ||
| Hyperparathyroidism | X | X | ||
| Hyperthyroidism and thyrotoxicosis | X | X | X | |
| Hypertriglyceridemia | X | X | X | |
| Hypoparathyroidism | X | X | ||
| Hypothyroidism | X | X | X | X |
| Metabolic syndrome, obesity | X | X | X | X |
| Osteoporosis | X | X | X | |
| Primary adrenal insufficiency | X | X | ||
| Thyroid cancer | X | X | ||
| Thyroiditis | X | X | ||
| Type 1 diabetes mellitus, diabetic ketoacidosis | X | X | X | X |
| Type 2 diabetes mellitus, hyperosmolar hyperglycemic syndrome | X | X | X | X |
| Vitamin D deficiency | X | X | X |
| Acute epiglottitis | X | X | X | |
| Acute glaucoma | X | X | ||
| Acute pharyngitis | X | X | X | X |
| Acute/chronic otitis media | X | X | X | X |
| Acute/chronic sinusitis | X | X | X | X |
| Allergic rhinitis | X | X | X | X |
| Angioedema | X | X | X | |
| Aphthous ulcers | X | X | ||
| Blepharitis | X | X | X | |
| Cataract | X | X | ||
| Chalazion | X | X | X | |
| Conjunctivitis | X | X | X | |
| Corneal abrasion | X | X | X | |
| Corneal ulcer | X | X | X | |
| Dental pain/abscess | X | X | X | |
| Epistaxis | X | X | X | |
| Eustachian tube dysfunction | X | X | X | |
| Foreign body in ear | X | X | X | |
| Foreign body in eye | X | X | X | |
| Foreign body in nose | X | X | X | |
| Hearing loss | X | X | ||
| Hordeolum | X | X | X | |
| Hyphema | X | X | ||
| Labyrinthitis | X | X | ||
| Laryngitis | X | X | X | |
| Macular degeneration | X | |||
| Mastoiditis | X | X | X | |
| Meniere disease | X | X | ||
| Nystagmus | X | X | ||
| Ocular trauma | X | X | X | |
| Leukoplakia | X | X | X | |
| Orbital cellulitis | X | X | X | |
| Otitis externa (acute, malignant) | X | X | X | |
| Papilledema | X | X | ||
| Parotitis | X | X | X | |
| Peritonsillar abscess | X | X | X | |
| Retinal detachment | X | X | ||
| Retinal vascular occlusion | X | X | ||
| Retinopathy (diabetic, hypertensive) | X | X | ||
| Subconjunctival hemorrhage | X | X | ||
| Temporomandibular disorders | X | X | ||
| Tinnitus | X | X | ||
| Tympanic membrane perforation | X | X | X | |
| Vertigo | X | X | X |
| Acute cholecystitis | X | X | X | |
| Acute hepatitis | X | X | ||
| Acute liver failure | X | X | ||
| Acute pancreatitis | X | X | X | |
| Anal abscess/fistula | X | X | X | |
| Anal fissure | X | X | X | |
| Appendicitis | X | X | X | |
| Celiac disease | X | X | X | |
| Cholangitis | X | X | ||
| Cholelithiasis | X | X | X | |
| Chronic hepatitis | X | X | X | |
| Chronic pancreatitis | X | X | ||
| Cirrhosis | X | X | ||
| Colon cancer | X | X | X | |
| Constipation | X | X | X | X |
| Diverticulitis and diverticulosis | X | X | X | |
| Dysphagia | X | X | X | |
| Esophageal varices | X | X | X | |
| Esophagitis | X | X | X | |
| Fecal incontinence | X | X | X | |
| Food allergies | X | X | X | |
| Food intolerances (gluten, lactose) | X | X | X | |
| Foreign body ingestion | X | X | X | |
| Gastritis | X | X | X | |
| Gastroesophageal reflux disease | X | X | X | X |
| Gastrointestinal bleeding | X | X | X | |
| Hemorrhoids (internal, external) | X | X | X | |
| Hernias | X | X | X | |
| Infectious diarrhea | X | X | X | |
| Inflammatory bowel disease | X | X | X | |
| Intussusception | X | X | ||
| Irritable bowel syndrome | X | X | X | |
| Ischemic bowel disease | X | X | ||
| Large-bowel obstruction | X | X | ||
| Nonalcoholic fatty liver disease | X | X | X | |
| Noninfectious diarrhea | X | X | X | |
| Pancreatic cancer | X | X | X | |
| Peptic ulcer disease | X | X | X | |
| Pyloric stenosis | X | X | ||
| Small-bowel obstruction | X | X | X | |
| Toxic ingestion (caustic substances, medications) | X | X | X | |
| Toxic megacolon | X | X |
| Acute prostatitis | X | X | X | |
| Bacterial cystitis | X | X | X | X |
| Benign prostatic hyperplasia | X | X | X | |
| Bladder cancer | X | X | ||
| Chronic prostatitis | X | X | ||
| Epididymitis | X | X | X | |
| Hydrocele and varicocele | X | X | ||
| Interstitial cystitis | X | X | ||
| Nephrolithiasis and urolithiasis | X | X | X | |
| Orchitis | X | X | X | |
| Overactive bladder | X | X | X | |
| Paraphimosis/phimosis | X | X | ||
| Prostate cancer | X | X | X | |
| Testicular cancer | X | X | ||
| Testicular torsion | X | X | X | |
| Urethritis | X | X | X | |
| Urinary incontinence | X | X | X |
| Acute/chronic lymphocytic and myeloid leukemia | X | X | ||
| Anemia of chronic disease | X | X | ||
| Folate deficiency anemia | X | X | X | |
| Hemolytic anemia | X | X | ||
| Hodgkin lymphoma | X | X | ||
| Hypercoagulable states (pregnancy-induced, trauma, COVID-19, DVT, Factor V Leiden) | X | X | ||
| Hypocoagulable states | X | X | ||
| Immune thrombocytopenic purpura | X | X | ||
| Iron deficiency anemia | X | X | X | X |
| Non-Hodgkin lymphoma | X | X | ||
| Sickle cell anemia | X | X | ||
| Vitamin B12 deficiency anemia | X | X | X |
| Candidiasis | X | X | X | |
| Chlamydial infections | X | X | X | |
| Coronavirus infections | X | X | X | |
| Epstein-Barr virus infections | X | X | X | |
| Gonococcal infections | X | X | X | |
| Herpes simplex virus infection | X | X | X | |
| HIV infection | X | X | ||
| Human papillomavirus infections | X | X | X | |
| Influenza | X | X | X | |
| Malaria | X | X | ||
| Measles | X | X | ||
| Mumps | X | X | ||
| Rabies | X | X | ||
| Respiratory syncytial virus infection | X | X | X | |
| Rubella | X | X | ||
| Septic disorders (sepsis, septic shock, systemic inflammatory response syndrome) | X | X | X | |
| Syphilis | X | X | X | |
| Tetanus | X | X | ||
| Tick-borne diseases (Lyme disease, Rocky Mountain spotted fever, anaplasmosis) | X | X | X | |
| Tuberculosis | X | X | X | |
| Varicella-zoster virus infections (chickenpox, herpes zoster) | X | X | X |
| Acute osteomyelitis | X | X | X | |
| Avascular necrosis | X | X | ||
| Bursitis | X | X | X | |
| Carpal tunnel syndrome | X | X | X | |
| Compartment syndrome | X | X | X | |
| Fibromyalgia | X | X | ||
| Fractures and dislocations | X | X | X | |
| Ganglion | X | X | ||
| Gout and psuedogout | X | X | X | |
| Inflammatory arthropathy (rheumatoid arthritis [including juvenile], psoriatic arthritis) | X | X | ||
| Lateral/medial epicondylitis | X | X | X | |
| Osgood-Schlatter disease | X | X | ||
| Osteoarthritis | X | X | X | |
| Rotator cuff tear | X | X | X | |
| Scoliosis | X | X | ||
| Septic arthritis | X | X | X | |
| Slipped capital femoral epiphysis/congenital hip dysplasia | X | X | ||
| Spinal disk herniation | X | X | X | |
| Spinal stenosis | X | X | ||
| Sprain and strain injuries | X | X | X | |
| Systemic lupus erythematosus | X | X | ||
| Temporal arteritis (giant cell arteritis) | X | X | X | |
| Tendinitis (infectious, non-infectious) | X | X | X |
| Bell palsy | X | X | X | |
| Cauda equina syndrome | X | X | ||
| Cerebral aneurysm | X | X | ||
| Delirium | X | X | ||
| Encephalopathy | X | X | ||
| Essential tremor | X | X | X | |
| Headache disorders (cluster headache, migraine, tension headache, pseudotumor cerebri) | X | X | X | |
| Hydrocephalus | X | |||
| Major neurocognitive disorder and dementia | X | X | ||
| Meningitis and encephalitis | X | X | ||
| Neuromuscular disorders (Guillain-Barre syndrome, myasthenia gravis, multiple sclerosis, amyotrophic lateral sclerosis, muscular dystrophy, botulism, Parkinson disease) | X | X | ||
| Peripheral neuropathy | X | X | X | |
| Radiculopathy | X | X | X | |
| Seizure disorders | X | X | X | |
| Stroke and transient ischemic attack | X | X | X | X |
| Syncope | X | X | X | |
| Traumatic brain injury (intracranial hemorrhage, concussion, post-concussion syndrome) | X | X | X |
| Abuse and neglect (child abuse, adult abuse, spouse or partner abuse) | X | X | X | |
| Acute stress disorder | X | X | X | |
| Adjustment disorders (bereavement and grief reaction) | X | X | X | |
| Anxiety disorders (generalized anxiety disorder, panic disorder) | X | X | X | X |
| Bipolar disorders | X | X | ||
| Depressive disorders (major depressive disorder, major depressive disorder with peripartum onset, major depressive disorder with seasonal pattern, post-partum) | X | X | X | X |
| Disruptive, impulse-control, and conduct disorders (oppositional defiant disorder, conduct disorder) | X | X | ||
| Feeding and eating disorders (anorexia nervosa, bulimia nervosa, binge-eating disorder, mixed disorder) | X | X | ||
| Neurodevelopmental disorders (autism spectrum disorder, attention-deficit/hyperactivity disorder) | X | X | ||
| Non-substance-related addictive disorders | X | X | ||
| Obsessive-compulsive disorder | X | X | ||
| Post-traumatic stress disorder | X | X | X | |
| Schizophrenia | X | X | ||
| Substance use disorders (illicit substances, prescription drugs, alcohol, tobacco) | X | X | X | |
| Suicide/homicide (risk, attempt, ideation) | X | X | X |
| Acute bronchiolitis |
X |
X |
X |
|
| Acute bronchitis |
X |
X |
X |
|
| Acute respiratory distress syndrome |
X |
X |
X |
|
| Hypersensitivity reactions (allergies, anaphylaxis) |
X |
X |
X |
|
| Asthma |
X |
X |
X |
X |
| Chronic obstructive pulmonary disease (chronic bronchitis, emphysema, chronic obstructive asthma) |
X |
X |
X |
X |
| Croup |
X |
X |
X |
|
| Cystic fibrosis |
X |
X |
||
| Foreign body aspiration |
X |
X |
X |
|
| Lung cancer |
X |
X |
X |
|
| Pertussis |
X |
X |
X |
|
| Pleural effusion |
X |
X |
X |
|
| Pneumonia (bacterial, fungal, viral) |
X |
X |
X |
X |
| Pneumothorax |
X |
X |
X |
|
| Pulmonary embolism |
X |
X |
X |
X |
| Pulmonary hypertension |
X |
X |
||
| Pulmonary nodules |
X |
X |
||
| Sleep apnea |
X |
X |
X |
| Acute kidney injury (prerenal, postrenal, intrinsic, rhabdomyolysis) | X | X | X | |
| Chronic kidney disease | X | X | X | X |
| Electrolyte abnormalities | X | X | X | |
| Pyelonephritis | X | X | X | |
| Renal cell carcinoma | X | X |
| Abnormal uterine bleeding | X | X | X | |
| Abruptio placentae | X | X | ||
| Amenorrhea | X | X | X | |
| Breast abscess and mastitis | X | X | X | |
| Breast cancer | X | X | X | |
| Cervical cancer | X | X | X | |
| Dysmenorrhea | X | X | X | |
| Ectopic pregnancy | X | X | X | |
| Endometriosis | X | X | ||
| Fertility issues (contraception) | X | X | X | |
| Gestational diabetes | X | X | ||
| Hypertension disorders during the perinatal period | X | X | X | |
| Normal pregnancy (medication use during the perinatal period, prenatal diagnosis/care) | X | X | X | |
| Menopause | X | X | X | |
| Ovarian cancer | X | X | ||
| Ovarian cysts | X | X | ||
| Ovarian torsion | X | X | X | |
| Pelvic inflammatory disease | X | X | X | X |
| Pelvic organ prolapse | X | X | ||
| Placenta previa | X | X | ||
| Postpartum hemorrhage | X | X | X | |
| Pregnancy loss | X | X | ||
| Premature rupture of membranes | X | X | ||
| Premenstrual syndrome | X | X | X | |
| Rh incompatibility | X | X | X | |
| Sexual dysfunction | X | X | X | |
| Uterine masses (fibroids, uterine cancers) | X | X | ||
| Vaginitis | X | X | X |
PANRE Practice Questions Based on the NCCPA Blueprint
The UWorld PA QBank reflects the NCCPA’s PANRE blueprint to simplify exam prep. It’s developed with your busy schedule in mind, and features high-yield questions written by practicing PAs to ensure you get the most realistic and up-to-date information possible. Try a few questions for free and read our detailed explanations.
A 1-month-old boy is evaluated for poor feeding. When nursing, the patient becomes diaphoretic, and, for the past week, he has fed for only 5 minutes at a time before falling asleep. Today, his weight is 30 g (1 oz) below birth weight. Vital signs are normal. Examination shows a thin infant who is sleeping but easily arousable. Cardiac examination demonstrates tachycardia with a 1/6 holosystolic murmur over the left lower sternal border and diastolic rumble over the cardiac apex. S2 is prominent. The patient is tachypneic, but lung fields are clear to auscultation. There is no clubbing, cyanosis, or peripheral edema. Which of the following is the most likely cause of this patient's symptoms?
| A. Atrial septal defect | ||
| B. Mitral stenosis | ||
| C. Tetralogy of Fallot | ||
| D. Transposition of the great vessels | ||
| E. Ventricular septal defect |
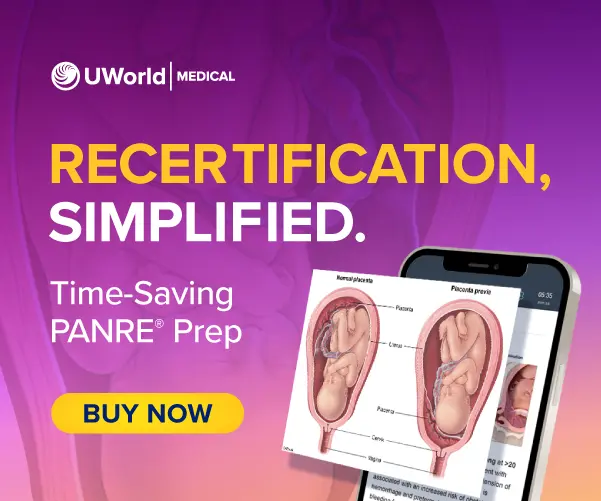
This patient's examination is most consistent with a large ventricular septal defect (VSD), a common congenital heart malformation. VSDs range from small and asymptomatic to large with significant left-to-right shunting. Features include the following:
- The characteristic murmur is holosystolic at the left lower sternal border. Small or moderate VSDs produce louder holosystolic murmurs due to turbulence. In contrast, large VSDs are quieter due to lower resistance (and less turbulence) through a larger orifice.
- An apical diastolic rumble may also be heard from increased flow across the mitral valve (as a result of increased left-to-right shunting across the VSD).
- As right ventricular pressure increases (due to increased flow), the S2 becomes more prominent (due to increased pressure closing the pulmonary valve).
Significant left-to-right shunting results in pulmonary overcirculation and pulmonary hypertension, growth failure, diaphoresis, easy fatigability, and congestive heart failure. Unrepaired, large VSDs result in permanent pulmonary hypertension, which leads to shunt reversal (ie, right to left rather than left to right) with cyanosis (Eisenmenger syndrome). Echocardiography confirms the defect's size and location. Treatment of large VSDs generally combines medications (eg, diuretics) and defect closure.
(Choice A) A large atrial septal defect can cause tachypnea. However, it would lead to a widened and fixed S2, which is not present in this patient.
(Choice B) Mitral stenosis also causes an apical diastolic rumble but not a holosystolic murmur at the left lower sternal border.
(Choice C) Tetralogy of Fallot consists of a VSD, right ventricular outflow tract obstruction (eg, pulmonic stenosis), overriding aorta, and right ventricular hypertrophy. The pulmonary stenosis component causes a harsh systolic ejection murmur at the left upper sternal border.
(Choice D) Transposition of the great vessels is characterized by the aorta arising from the right ventricle and the pulmonary artery arising from the left ventricle. It would cause cyanosis, which is not seen in this patient.
Educational objective:
Large ventricular septal defects cause growth failure, pulmonary hypertension, and heart failure. They classically produce a holosystolic murmur that is loudest at the left lower sternal border and an apical diastolic rumble due to increased blood flow across the mitral valve.
A 68-year-old man comes in due to 2 months of bulky, foul-smelling diarrhea. The patient reports that his stools appear oily in character and are difficult to flush. He has also had intermittent, epigastric abdominal pain for the past 6 months that has not improved with a proton pump inhibitor trial. The patient has had no melena, nausea, or vomiting, but he has lost 7 kg (15.4 lb) over the last 6 weeks. He drinks 5 or 6 beers daily and has a 20-pack-year history. On physical examination, the epigastrium is mildly tender to palpation but is without distension, rebound tenderness, or guarding. Which of the following is most likely to establish the diagnosis in this patient?
| A. Anti–tissue transglutaminase antibodies | ||
| B. CT scan of the abdomen | ||
| C. Lactose breath hydrogen test | ||
| D. Serum amylase | ||
| E. Upper gastrointestinal endoscopy |
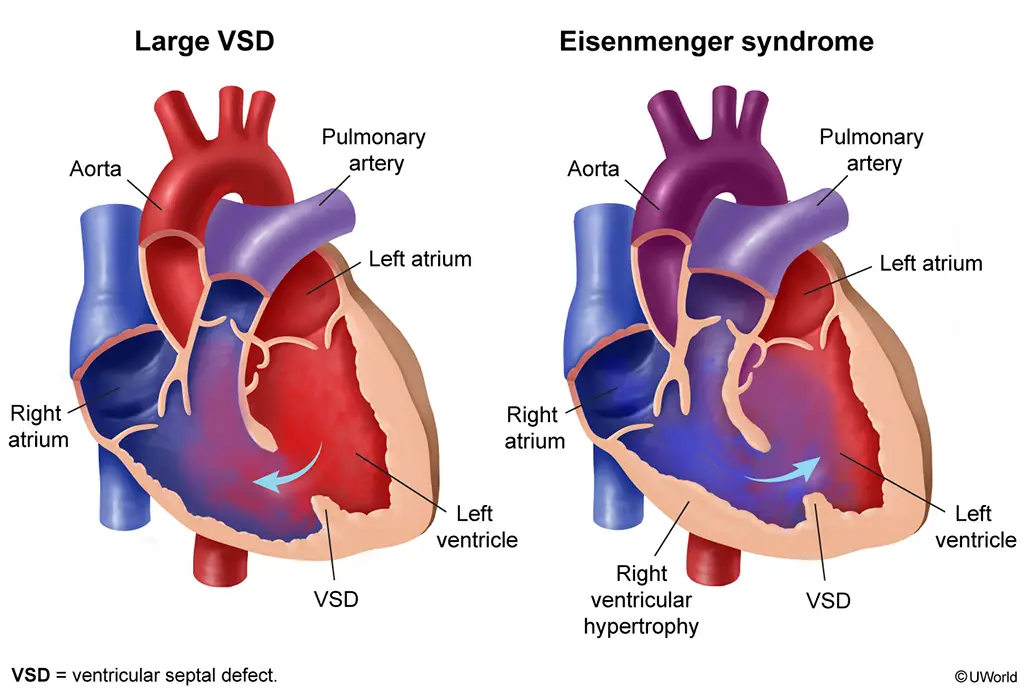
This patient's weight loss, abdominal pain, and steatorrhea (bulky, oily, foul-smelling stools often difficult to flush) are suggestive of chronic pancreatitis, defined as progressive pancreatic inflammation with permanent structural damage and resultant endocrine and exocrine dysfunction. Risk factors for chronic pancreatitis include alcohol use (most common), genetics (eg, cystic fibrosis), pancreatic ductal obstruction (eg, malignancy, stones), and autoimmune disease. Patients usually have episodic or daily abdominal pain and findings of pancreatic insufficiency (eg, malabsorption, diabetes mellitus).
Pancreatic fibrosis leads to decreased enzyme levels within the pancreas; as a result, serum amylase and lipase levels are usually normal and nondiagnostic (Choice D). Plain abdominal radiographs reveal calcifications within the pancreatic duct in only 30% of patients. Abdominal CT scan and MR cholangiopancreatography are the preferred diagnostic modalities because they are more sensitive and can readily show calcifications, dilated ducts, pancreatic atrophy, or fluid collections (pseudocyst). Treatment involves pancreatic enzyme replacement, which includes lipase to aid in fat digestion and improve steatorrhea.
(Choice A) Anti–tissue transglutaminase antibodies are present in celiac disease, which is due to gluten enteropathy and may be associated with an increased risk for chronic pancreatitis. Celiac disease can be asymptomatic or present with steatorrhea, weight loss, iron deficiency anemia, nutritional deficiencies (eg, vitamins D and B12), and metabolic bone disease. However, it usually does not cause significant abdominal pain, as seen in this patient.
(Choice C) Lactose breath hydrogen testing aids in the diagnosis of lactose intolerance, which typically presents with abdominal pain, bloating, flatulence, and diarrhea (eg, bulky, frothy, watery stools) following lactose ingestion (eg, milk). Weight loss is atypical, and this patient's alcohol intake makes chronic pancreatitis more likely.
(Choice E) Upper gastrointestinal endoscopy can effectively diagnose gastric, duodenal, and esophageal pathology (eg, malignancy, ulcers, inflammation). However, this patient has no evidence of dysphagia, vomiting, or melena to suggest an upper gastrointestinal disorder.
Educational objective:
Chronic pancreatitis usually presents with episodic or daily abdominal pain and findings of pancreatic insufficiency (eg, diabetes mellitus, steatorrhea, weight loss). Chronic alcohol consumption is the most associated risk factor. Diagnosis is typically confirmed with abdominal CT scan or MR cholangiopancreatography showing calcifications, dilated ducts, and pancreatic atrophy.
- Pancreatitis
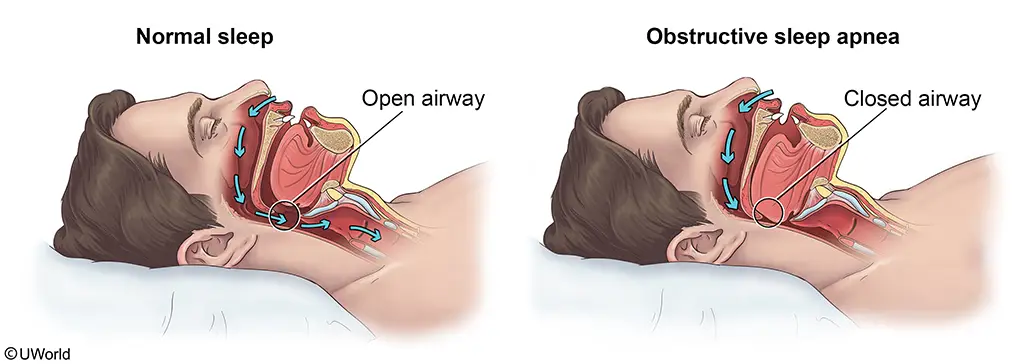
A 54-year-old man comes to the office due to daytime sleepiness and lack of energy. The symptoms began 6 months ago and have progressively worsened so that he feels "completely drained" by the end of the day. The patient's wife mentions that he snores loudly. He has not had a medical evaluation in over 10 years. BMI is 34 kg/m2. Physical examination shows a narrow oropharynx and a large neck circumference. This patient is at increased risk of developing which of the following?
| A.Bronchiectasis | ||
| B. Hypertrophic cardiomyopathy | ||
| C. Laryngeal carcinoma | ||
| D. Narcolepsy | ||
| E. Pulmonary hypertension |
This patient, an obese man with loud snoring, daytime sleepiness, and suggestive examination findings (eg, thick neck, narrow airway) most likely has obstructive sleep apnea (OSA). OSA is characterized by recurrent obstruction of the upper airway during sleep; each nocturnal episode of reduced ventilation causes transient hypercapnia and hypoxemia. These blood gas derangements result in reflexive systemic and pulmonary vasoconstriction, endothelial dysfunction, abnormal venous return and cardiac output, and sympathetic cardiac stimulation.
Prolonged, untreated OSA can cause pulmonary hypertension and right heart failure. Most patients with OSA will develop systemic hypertension due to chronic sympathetic stimulation and elevated plasma norepinephrine levels. Patients also lose the normal diurnal variation in blood pressure. Other cardiovascular complications of OSA include atrial fibrillation and other arrhythmias, coronary artery disease, and increased risk of sudden cardiac death.
(Choice A) Acquired bronchiectasis may be seen in patients with recurrent infection, impaired drainage (eg, cystic fibrosis), or airway obstruction (eg, foreign body aspiration.
(Choice B) Systemic hypertension, as seen in OSA, can lead to mild-to-moderate left ventricular hypertrophy and impaired systolic and diastolic function. In contrast, hypertrophic cardiomyopathy is an autosomal dominant disease of the cardiac sarcomere characterized by severe myocardial hypertrophy. It is not associated with hypertension or OSA.
(Choice C) Laryngeal carcinoma is associated with cigarette smoking and heavy alcohol use.
(Choice D) Like OSA, narcolepsy can also cause daytime drowsiness. However, narcolepsy is also associated with cataplexy (sudden loss of muscle tone), sleep attacks, sleep paralysis, and hypnagogic hallucinations. OSA is not a risk factor for narcolepsy.
Educational objective:
Obstructive sleep apnea presents in obese individuals with excessive daytime sleepiness and signs of nocturnal upper airway obstruction (eg, snoring, gasping). The condition is associated with systemic hypertension. Prolonged, untreated obstructive sleep apnea can also cause pulmonary hypertension and right heart failure.
- Sleep disorders